Полная версия
Low Blood Sugar: The Nutritional Plan to Overcome Hypoglycaemia, with 60 Recipes
Self-diagnosis is therefore not advisable; a naturopath or sympathetic doctor should be able to offer more objective diagnostic methods. These can include, in addition to detailed case-history taking, the six-hour glucose tolerance test, the measurement of adrenal and thyroid hormones and a blood insulin test (these will be discussed in due course).
At some time in their lives most people experience one or more of the symptoms listed above. They are usually caused by transient low blood sugar – a temporary or passing fall in the blood sugar level. This is rapidly rectified by the body’s own sugar regulation mechanism. Once a balance is achieved, the symptoms usually disappear. If, however, there is a chronic imbalance in our sugar regulation, the symptoms may well improve or change, but they will always return if the actual imbalance is not corrected.
Now let us look more closely at the way in which a drop in the blood sugar directly affects the various organs and systems of the body, giving rise to the symptoms outlined. In this way you will begin to understand why the blood sugar level is so important to the normal running of the body. The effects of low blood sugar can be classified as follows:
Nervous system changes
The main nutrient needed by the nervous system is glucose. There is no really adequate substitute and, although other substances are involved, they cannot replace glucose. Unfortunately, it is not fully understood just how glucose acts on the nervous system, but it has been noted that when a healthy patient is injected with insulin (the opposite of glucose), profound and sudden changes in the efficiency of the nervous system occur within minutes. This is completely reversed by an injection of glucose. This tends to confirm that the nervous system requires a continuous supply of glucose in order to function efficiently.
Although the weight of an adult brain is only two per cent of the total body weight, the activity of the brain, in terms of utilization of glucose, may amount to 20–25 per cent of the total body activity. In spite of this, the total amount of glucose concentrated within the brain at any one time would, under normal conditions, be exhausted in 10–15 minutes. The effects of glucose starvation on the brain and nerve tissue as a result of a low level of blood sugar are as follows:
1 Insufficient oxygen.
2 Reduction in specific substances within the brain that are essential for nervous activity.
Let us look at the symptoms that can result from such changes.
CIRCULATORY CHANGES
Not surprisingly, the system first affected by a drop in the blood sugar level is the blood circulatory system. This, of course, includes the heart and blood vessels. When the blood sugar falls, the body automatically reacts in an attempt to restore balance to the system. This response involves the release of adrenaline from the adrenal glands, to raise the blood sugar. Adrenaline is also released in stressful situations. This means that if an individual has persistent low blood sugar, they may have symptoms similar to those produced by chronic stress. These can include:
1 An irregular increase in the heart rate, causing palpitations and breathing difficulties.
2 Angina-like symptoms involving a reduction in circulation to the heart muscle, chest cramp and pain in the chest and arms.
3 A general withdrawal of blood to deal with the ‘stress effects’, causing coldness of the hands and feet, muscular cramp and a poor adaptation to temperature changes.
GLANDULAR CHANGES
The changes involved in the glandular system following a drop in the blood sugar level are widespread and could well provide sufficient material for another book. However, in this context, it is adequate simply to briefly look at the glands affected.
1 Pituitary gland. This is the master control gland influencing the thyroid and adrenal glands.
2 Adrenal glands. These glands produce adrenaline, cortisol (hydrocortisone), DHEA and other hormones. It is the persistent stimulation of these glands in a patient suffering from low blood sugar that provides the causative link between blood sugar and rheumatoid arthritis. Overactivity, with subsequent exhaustion of the adrenal glands, can cause a reduction in the availability of cortisol and the ‘mother’ hormone DHEA, which provide protection against joint pain and inflammation.
3 Thyroid gland. Changes that occur with thyroid activity are of less significance than other glands. Although, like the adrenal and pituitary glands, the thyroid secretions are essentially antagonistic to insulin and thus thyroid imbalance can contribute to a blood sugar imbalance. A vicious cycle may be established whereby a mildly deficient thyroid causes low blood sugar and the subsequent adrenal stress can further depress the thyroid.
DIGESTIVE CHANGES
The changes in gastric (stomach) activity that occur with low blood sugar are mainly caused by the increased insulin level in the blood, rather than the actual deficiency of blood sugar. A standard hospital test to assess the efficiency of digestive activity involves administering to the patient an injection of insulin. This prompts a rapid and predictable increase in the amount of stomach acids, which are then measured. It follows that if this test has such an effect, the fluctuations of the insulin level in the blood – as occurs in low blood sugar and insulin resistance – would have a similar effect. Indeed, in practice, I find that many patients suffering from stomach ulcers, heartburn, hiatus hernia and other digestive ailments frequently have an underlying blood sugar imbalance.
Those with food intolerances may suffer symptoms that are partially caused by low blood sugar. Unfortunately, as a result of symptom similarity the two conditions are often confused.
PSYCHOLOGICAL CHANGES
As I discussed previously, changes in blood sugar can have a significant impact on the brain and nervous system – it is hardly surprising then that many patients suffering from low blood sugar also have personality problems. The most common symptoms found in low blood sugar patients are depression, anxiety and mental confusion. Many researchers, particularly in the US, consider chronic low blood sugar to be a contributing factor in such serious personality problems as schizophrenia and manic depression (bipolar disorder).
We know that low blood sugar can lead to fatigue of the adrenal glands, and that the adrenal glands are the body’s main defence mechanism against stress. It therefore seems likely that those with chronic low blood sugar can suffer a vicious circle of adrenal exhaustion, which causes anxiety, and with the anxiety comes further exhaustion and stress. Unfortunately, many people suffering from stress often overeat or comfort-eat the wrong foods. They also tend to miss meals, relying on caffeine, tobacco and alcohol for their fuel, thus further aggravating any blood sugar imbalance.
Respiratory changes
Surprising as it may seem, low blood sugar can also affect the respiratory system. The reason for this is a substance called histamine. This compound is naturally present in all the cells of the body and has a variety of uses – not least is its role in controlling osmosis (passage of water) between the body membranes. It is well known that if the histamine level increases, the characteristic symptoms can include hay fever, skin rashes and asthma. The link between histamine and the blood sugar exists because histamine and glucose are on separate ends of a seesaw. If the glucose level drops, the histamine level rises and vice versa. It follows that a patient who has low blood sugar may, under certain conditions, also have asthma or hay fever.
It is an interesting fact that diabetic patients rarely develop asthma; there are also very few cases on record of an asthma patient also having diabetes. (The main exception is the condition known as cardiac asthma, which is associated with heart disease). Many asthma patients find to their delight in their late 40s and 50s that their asthma symptoms improve. The reason for this is that they are developing late onset diabetes and their blood sugar has become raised above normal level, thus protecting them from asthma.
It should be said that low blood sugar is not the only cause of asthma; there are certain types of asthma caused by stress or extreme sensitivity to various allergens, vigorous exercise, infections and various irritant particles. A good medical dictionary will list more than 30 different types of asthma, usually defined according to their cause.
Musculo-skeletal changes
The other system of the body that is frequently affected by low blood sugar is the musculo-skeletal system – in other words, the muscles and joints. As already explained, the effect of the adrenal glands and, in particular, Cortisol on joint inflammation is well documented, hence the apparently miraculous symptom-relief afforded to rheumatoid arthritis patients when Cortisol is taken or injected. If the adrenal glands are overworked and fatigued as a result of prolonged low blood sugar, and the efficiency of steroid hormones that protect the joints from inflammation is compromised, joint pain, stiffness and swelling may result. This link between musculo-joint symptoms and stress is known to all of us. The expressions ‘pain in the neck’ or ‘pain in the butt’ illustrate the connection. Whether any adrenal exhaustion is caused by stress alone or indirectly caused by low blood sugar, the resulting joint and muscle symptoms are the same.
General symptoms of low blood sugar – the two stages
STAGE ONE SYMPTOMS – FALLING BLOOD SUGAR
The immediate symptoms that follow a fall in blood sugar result from a reduction in the brain and nervous system fuel (i.e. glucose). These first stage symptoms generally include mental and physical lethargy, partial or total loss of concentration, headaches, trembling and/or dizziness, a tendency to yawn, paleness of lips and face with either a skin coldness or heat with perspiration, unexplained anxiety and a sudden urge for chocolate or anything sweet.
STAGE TWO SYMPTOMS – ADRENAL COMPENSATION
The second stage symptoms are caused by the adrenal response to the low blood sugar level. For many people these symptoms are more distressing than those of the first stage.
The surge of adrenaline that occurs in response to low blood sugar causes symptoms identical to the body’s response to stress. The metabolism is literally revved up for action. The heart rate increases and the blood flow to muscles is stepped up. This can be likened to pulling out the choke on a car to increase the available fuel. Heavy sweating can occur, with breathlessness and unpleasant palpitations.
A frequent consequence of the stress reaction is a degree of irritability or even aggression – a good example being the mood swings of the diabetic patient. Those readers who have a diabetic friend or relative will know only too well that when a ‘hypo’ occurs the victim becomes both irritable and aggressive. Many people with low blood sugar symptoms show a degree of anxiety, irritability or depression – symptoms that often improve as their problem is resolved.
All this is part of our body’s normal reaction to stress. If we are confronted by an angry bull as we cross a field we need to increase our oxygenation, heart rate and muscle strength to hastily flee. Most athletes and competitive sports people know the value of this adrenaline effect, for the power and speed increase it can provide. They learn to control and at times to override the adrenal response to further their sporting goals.
For most of us this alarm-response by our body is in direct proportion to the intensity of the threat or stress. However, many who suffer with chronic low blood sugar lose their fine control and an adrenal hair-trigger response to stress of any kind leads to frequent and often unnecessary alarm-responses. When adrenaline is released on a regular basis for trivial reasons, many distressing symptoms can develop. Some sufferers, for instance, are frequently awakened at 3–4am bathed in sweat, anxious, with a rapid pulse and short of breath. This occurs because the adrenal response to their nocturnal low blood sugar is being inappropriately triggered and their metabolism is stressed.
Unfortunately, even when we sleep changes in the blood sugar can activate the adrenal response. Professor Hans Selye, who wrote the definitive first description of our response to stress in his landmark 1956 book The Stress of Life, described sleep as follows: ‘No one is ever absolutely at rest, while alive. Even during sleep, your heart, your respiratory muscles, your brain continue to work. It makes no difference that you are not conscious of this and that these activities require no voluntary effort on your part’.
Our management of stress is a very individual quality that depends on many factors. The amount and type of activity appropriate to a five-year-old child would be very stressful for a 75-year-old man and vice versa. Our stress load and our stress handling are unique to each of us. Stress can, of course, be on many levels, psychological, chemical, structural or environmental. It does not always need to be unpleasant or unexpected to give rise to symptoms. Enjoyable, planned events can also be stressful – excited children becoming sick at parties and sports people suffering asthma attacks are examples of this.
Trigger factors
The most common triggers that can cause low blood sugar symptoms include one or more of the following:







CHAPTER 4 The diagnosis of low blood sugar
I have diagnosed and treated patients with low blood sugar for 35 years, and over this time I have learnt that a simple diagnosis of ‘low blood sugar’ is rarely helpful for the patient and not always accurate. Indeed the diagnostic challenge with low blood sugar symptoms is to provide satisfactory answers to the following questions:
1 Are the symptoms of low blood sugar seen in a patient the result of poor stress handling or a faulty diet, and therefore transient and probably reversible? or
2 Are the symptoms the result of a chronic glandular imbalance, long-term stress, excessive reliance on caffeine, tobacco, alcohol and other drugs, or the many other factors associated with dysglycaemia?
In fact, many people with the symptoms of low blood sugar have several causes running parallel. As low blood sugar masquerades as so many different conditions, and can create such a diversity of symptoms, diagnosis can be difficult. For this reason, and others that will be discussed later, it is not wise to diagnose low blood sugar without professional help. Low blood sugar mimics very many serious diseases and it is therefore essential that the possibility of more serious causes for the symptoms is ruled out.
The clinical diagnosis of low blood sugar falls naturally into several stages.
Family history
Low blood sugar disorders can pass from generation to generation. It therefore follows that a detailed evaluation of a person’s family health is of considerable diagnostic value.
Table 1 – The family connection, 25 patients
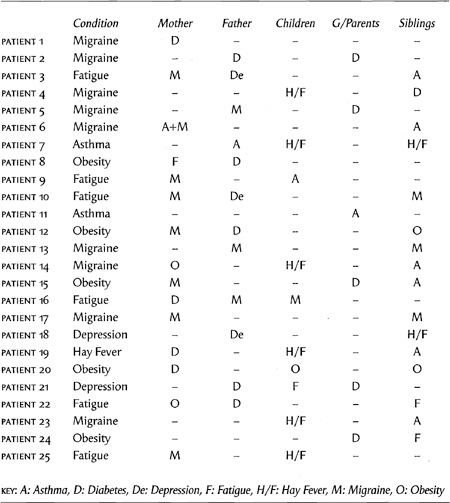
Table 1 illustrates the family history of 25 patients with confirmed low blood sugar. These patients have been selected because they are typical low blood sugar cases. You will see that characteristic disorders pass through each family. The majority of patients with low blood sugar symptoms tend to show a previous history in their family of either asthma, migraine, hay fever, diabetes, obesity, chronic fatigue or depression.
Present symptoms
As we know, the symptoms of low blood sugar can be misleading to the diagnostician. Often of more significance than a list of symptoms are the pattern of cause and the time of onset of symptoms. One patient, Mr A, may experience headaches when reading or watching television, while another patient, Mr B, may develop headaches only in the early morning or when he drinks certain types of wine. In the case of Mr A, he may well have eyestrain, but Mr B could be suffering from low blood sugar.
Fatigue at the end of the day may be caused by overwork, anaemia or a variety of ailments. Fatigue on rising, which improves towards the end of the day, offers a strong clue to the possible diagnosis of low blood sugar. A subjective evaluation is never easy, for unless one is familiar with the diagnostic value of symptom patterns, it is very difficult to diagnose one’s own problems.
One of the chief characteristics of low blood sugar sufferers is the combination of physical and mental symptoms coupled with considerable variation in the symptoms. Sometimes the patient may feel on top of the world; at other times he or she may feel exhausted and depressed for no apparent reason. Remember, we are not dealing with a predictable organic disease such as arthritis or anaemia, but an imbalance in the nervous, circulatory, digestive and endocrine systems. Therefore any symptoms may be the expression of a great number of interrelating and fluctuating causes. These causes can include diet, emotional state, menstruation, time of day, stress, fatigue, the side effects of drugs and many other factors.
Past health
No illness suddenly arrives. There are always changes in the body before the symptoms become apparent to the patient. With low blood sugar the early symptoms are usually vague and difficult to identify. The commonest symptoms are fatigue associated with a dulling of concentration, irritability and mild anxiety or depression, feeling thick-headed on waking and a distinct loss of zest before mid-morning.
Early symptoms may also include transitory feelings of panic or breathlessness with cold sweating and headaches, often accompanied by a craving for something sweet. Such symptoms are often diagnosed as being due to overwork, stress or just ‘nerves’. The usual sedatives and relaxants are prescribed, but if symptoms are caused by low blood sugar, any relief will be only temporary. The fatigue will still be there, often without excessive effort or work, and the anxiety will persist, despite a lack of stress.
It is unfortunate that many people with low blood sugar suffer their symptoms because of a false diagnosis. Often they are classified by doctors and family as neurotic when, in fact, the cause of their symptoms is physiological and not psychological.
When looking into a person’s history, disorders often feature that provide clues to future low blood sugar. These include hepatitis, jaundice, morning sickness during pregnancy, biliousness and intolerance of fats, a history of gall bladder trouble, chronic fatigue and overweight. The role of the body’s early warning system is to indicate the development of a biochemical imbalance or damage of some kind. If the early symptoms of low blood sugar are accurately diagnosed before the obesity, fatigue, migraines and diabetes develop, a great deal of pain and distress may be avoided.
Dietary habits
Faulty nutrition is the single most important cause of low blood sugar. The modern Western diet, with its high sugar content, refined starches, artificial additives and low nutritional value, provides an appropriate formula for causing blood sugar imbalances. If we also consider the modern habits of snack meals, frequent coffees and the excessive use of drugs, alcohol, cola drinks and tobacco, it is no surprise that the incidence of high and low blood sugar conditions is increasing at an alarming rate.
As poor diet is a key factor in the development and maintenance of low blood sugar, it is obviously an important clue in the diagnosis of the problem. I find in practice that most low blood sugar sufferers have characteristic dietary habits that provide important leads to the cause of their symptoms. It must be remembered that, for these patients, meals are not simply a question of choice, for the pattern of meals and type of food is strongly influenced by the underlying low blood sugar. Sugary foods and drinks and caffeine-rich or alcohol-rich drinks all provide temporary relief to the symptoms of low blood sugar. Not surprisingly, the diet reflects this and is usually high in these items and in particular there may be cravings for sweet foods far in excess of normal consumption. One of the most significant clues is a person’s sugar intake – two to three teaspoonfuls in either tea of coffee is not unusual. Smoking can also be a clue, as many tobacco addicts experience low blood sugar symptoms.
Because our blood sugar is linked to the appetite, a frequent symptom is hunger. This is not a general feeling of hunger, but more often a craving for a certain type of food. However, the low blood sugar patient, because of the symptoms produced by his condition, often cannot face food. This usually occurs at breakfast time as the blood sugar drops overnight. The thought of breakfast can make a person with low blood sugar feel physically sick. Usually a coffee or cigarette starts the day, and the inevitable ‘high’ provided by the caffeine produces a mid-morning ‘low’ as the blood sugar drops again. So the day consists of small frequent ‘shots’ of sugar or caffeine to maintain the energy level and the concentration at a tolerable level.
When the blood sugar has sunk to a low level, usually around 3–5am, the low blood sugar sufferer often wakes with stomach cramp, indigestion or just hunger – for this reason they are often night nibblers.
The two diets listed below are those of two patients seen in my practice. Every characteristic of the typical eating habits associated with low blood sugar can be seen here.