Полная версия
Zita West’s Guide to Getting Pregnant
No, unfortunately saliva has been found to be quite detrimental to sperm. In laboratory conditions, sperm cannot swim if they are in contact with saliva or any other lubricant – either water – or oil – based – all of these have some effect on sperm motility (movement). Although this has not been tested in women (and would be quite hard to study!), one has to assume that the effect would be the same in the body. Saliva of course contains an enzyme, ptyalin, which starts the digestive process – digesting carbohydrates – so this is not good news for the sugars contained in sperm or their swimming fluids!
Lubricating gels block the sperm. Egg whites are protein and can trigger an allergic reaction in some women.
I don’t seem to have many secretions, yet they seemed plentiful when I was younger. Is this common?
Yes, as we get older the quantity and quality of our cervical secretions are reduced. This is one of the reasons why fertility rates are lower in older women. The other factor is often that when young we are often unaware of the significance of these secretions and may even be quite alarmed by them. Sometimes women feel the secretions are a sign of infection – or that they may have damaged themselves somehow.
It is also common for women to report that as soon as they start to look out for the secretions, they no longer seem to see them. The amount of secretions will vary from woman to woman and sometimes from one cycle to the next in the same woman. If you are having sex around your fertile time (which is of course pretty vital) then often some of your natural secretions will get mixed in with the seminal fluid, which then comes away a few minutes after you have sex (even if you are lying flat) and can give you the impression that you’ve fewer secretions than you really have.
What if I spot between periods?
This depends on when the spotting is occurring. The first thing to remember is that ANY unusual bleeding or spotting must be checked out by your doctor. It is important to keep your cervical smears up to date, as these check not only for pre – cancerous changes but also for signs of infection.
If any spotting has been checked out medically and you are told that there is no concern medically, the following information may be helpful. Some women get spotting towards the end of a period – this may be quite normal as the period dries up. Some women have spotting leading into a period. This should be recorded at the end of the cycle – with the new cycle (Day 1) starting on the first day that you notice fresh red bleeding. If you consistently get some spotting for a day or so before your red bleed starts (pre – menstrual spotting), this may be an indication that your progesterone level is falling and may require medical help.
Very occasionally women who are observing cervical secretions report slight spotting tingeing the wet stretchy secretions – this is nothing to be concerned about (provided you are having regular smear tests) and may simply be due to the fact that you are more aware of your secretions than ever before!
Some women notice a tiny spot or so of blood (or even more) around the time implantation is occurring – so this could be a very positive sign.
I seem to have a long cycle and have secretions nearly all of my cycle.
Although most women report that they are dry immediately after a period and when approaching the next period, some will observe secretions for most, if not all, of the cycle. Again, if you suspect any infection, get this checked by your doctor.
Quite a common reason for secretions throughout the cycle is a cervical eversion (where the inner lip of the cervix protrudes onto the outside of the cervix, causing an increase in the wetter type of secretions). This is more common after you have been on the Pill, or after pregnancy or miscarriage, and may go away of its own accord. See your doctor or practice nurse, who will be able to see if there are any signs of an eversion. It is not necessary to treat this, unless the secretions are causing trouble with increased wetness. Your doctor will be able to advise you.
Women can learn to distinguish cervical secretions more easily if they get expert help from a health professional trained in fertility awareness methods – such help can be found at www.fertilityuk.org.
When I take my temperature it seems to be very low, and never gets above 35.5°C. Is this a problem?
If your temperature does not seem to fit on the scale of the usual fertility chart, the most likely reason is either a faulty thermometer or inexperience in taking your temperature. It may be worth consulting a trained fertility practitioner. If you have a very low waking temperature – and you are sure you are taking it correctly – then do check this with your doctor. If you also have other symptoms such as tiredness, or are feeling the cold, then there may be a thyroid problem. Your doctor will be able to check your thyroid function as part of other hormone testing.
I suffer from PCOS and have very irregular cycles. How can I know when I should have sex?
This is difficult. Many women with PCOS have erratic ovulation and confusing fertility symptoms, and can have patchy secretions throughout the month due to erratic hormone levels. Ovulation kits will be of no value if your level of LH is raised or high, as it sometimes is when you have this condition.
Plan to have frequent, regular sex throughout the month. I have seen many women conceive with PCOS; the good news is 70 per cent conceive naturally and 20 per cent conceive with the help of appropriate medication.
If you are older, have been diagnosed with PCOS and have made all the necessary lifestyle changes, don’t leave it too long before you consult with your doctor about problems getting pregnant – it’s possible you may not be ovulating.
understanding male fertility
Male Reproductive Organs
A man’s general health is just as important to conception as a woman’s, although this often gets overlooked by fertility experts, who tend to be gynaecologists and obstetricians – specialists in female, not male, reproductive health. And your health is never more important than when you and your partner are trying to conceive. Very often, problems in conception are thought to be wholly the woman’s, but this is not the case. When a couple have a problem with conception, the problem is only with the woman in around 35 to 40 per cent of cases and with the man between 30 and 35 per cent of the time. Problems that arise from combined difficulties in both partners account for the other 25 to 35 per cent of cases.
I do think that, slowly, the message is getting through: The health of the sperm is just as important as a woman’s gynaecological health when it comes to conception. At our clinic we will offer a semen analysis straight away; if you focus all clinical attention on the woman, valuable fertility time may be wasted.
Unlike women, men do not have cycles which could alert them to the fact that there may be problems – so very often it can come as a real shock when the results of a semen analysis are poor. And semen analysis is only part of the story: the sperm may look fantastic but there may be infections or DNA fragmentation, which will not show up on semen analysis. Specimens sent to standard general microbiology or pathology labs may not receive immediate attention, and morphology assessment in particular (see page 286) may be inadequate, giving false or misleading results. We have seen this happen so many times.
Twenty-five per cent of male infertility remains unexplained. Sperm counts have been steadily declining over the last 50 years. Scientific evidence clearly points towards our constant exposure to toxins in our everyday modern lives, contributing to our reproductive downfall. These factors are known to affect male reproductive function seriously, and may well contribute to this high number of unexplained cases.
Insufficient emphasis is put on the contribution of lifestyle factors to sperm quality and male infertility. Infertility is multi – factorial and, in many cases, the severity of male infertility is exacerbated by lifestyle factors, which can and should be addressed to optimize whatever fertility potential there is. Even if the semen analysis is good, good sperm genetic health and metabolic fitness can always be improved by cutting down on the lifestyle factors that are known to harm the sperm, and eating a good healthy diet to reduce oxidative damage to the sperm.
Sperm Production
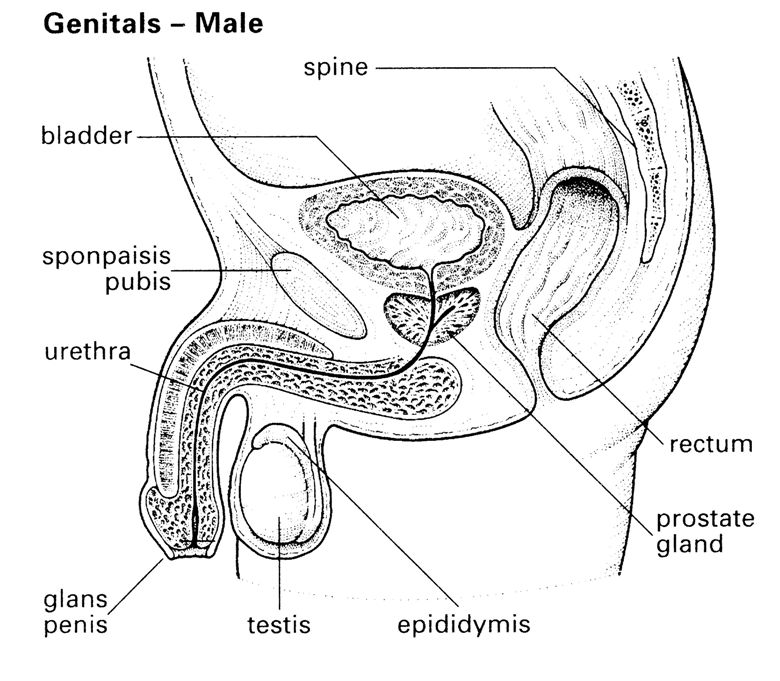
Sperm are produced in the seminiferous tubules of each testis. The two testes are contained in the scrotal sac, next to the penis. Unlike women, who are born with around 2 million immature eggs in their ovaries, although they don’t begin to mature and ovulation doesn’t occur until after puberty, a man doesn’t produce sperm at all until puberty, when his reproductive hormones become active.
Hormones are sometimes called the ‘chemical messengers’ of the body. Secreted by a gland in one part of the body, hormones are transported via the bloodstream to another area of the body, where they have an effect. At puberty, for both men and women, an area of the brain called the hypothalamus starts secreting gonadotrophin – releasing hormones, which cause the pituitary gland to produce two other hormones: follicle – stimulating hormone (FSH) and luteinizing hormone (LH). When these two hormones are produced, the gonads – testes in men, ovaries in women – are stimulated, to produce sperm in the man and to stimulate ovulation in a woman. The average age for male puberty is between 12 and 14, although this can vary quite widely and is influenced to some degree by genetic make – up, race and diet. Hormonal stimulation of the testes leads to the production of sperm and, as long as the necessary hormones are available and at the correct levels, and there is no disease or illness affecting production, this is a continuous process from puberty onwards.
The other effect of FSH and LH on the testes is to stimulate the production of testosterone, within the testes, responsible for the development of male characteristics like facial, armpit and pubic hair, and body hair in general. The voice also deepens as the testosterone makes the Adam’s apple at the front of the neck enlarge. Muscle tissue is increased and strengthened, and mood is also influenced – not least in promoting sexual interest. Some men seem to produce more testosterone than others, but this doesn’t mean they are more fertile than other men. Testosterone is responsible for the secondary sex characteristics described above, and isn’t particularly an indicator of the quality of sperm or a man’s fertility.
The process by which sperm are formed in the testes takes around 100 days – 74 for the sperm to develop, and then another 20–30 days to reach maturity, which is what you have to allow before you can expect to see any improvement in sperm quality or quantity. But as sperm production is happening continuously, a man is continuously fertile, unlike a woman who is only fully fertile for about eight hours during each one of her fertility cycles!
Within the testes, the sperm start their journey through the thousands of tiny, coiled seminiferous tubules. Sperm start as spermatocytes, primary cells that divide and develop into spermatids, which are immature, tail – less sperm. During their journey along the seminiferous tubules, where they are nourished by the sertoli cells that line the tubules, each spermatid grows a head that contains all the chromosomal material. Chromosomes carry all of a man’s genetic material ready to pass on to a child, including the chromosome (usually referred to as the sex chromosome) that decides whether a baby will be a boy or a girl. Whereas every one of a woman’s eggs contains the genetic material for a girl (the X chromosome), a man’s sperm will contain either an X chromosome or a Y chromosome (for a boy).
As well as growing a head during their 74-day development, the sperm form a middle piece that contains the energy source, and a tail. It is the mid – piece of the sperm, with its energy source, which is responsible for the tail’s ability to move and transport the sperm independently. Without a properly functioning tail, sperm may swim around in circles rather than forward in a straight line, or may not swim at all.
From the seminiferous tubules, the maturing sperm move into the epididymis, which is a long tube, around 18 feet in length but only a three – hundredth of an inch in diameter, which is coiled and situated at the back of the testicle.
Once produced, sperm then move up into the vas deferens, the tubes that eventually feed into the urethra and on through the penis, via the ejaculatory duct. Here, the sperm mix with secretions from the seminal vesicles and the prostate gland to form the seminal fluid. Once combined, the sperm and seminal fluid are referred to as semen. The secretions of the prostate gland are alkaline, which helps to neutralize the acidity of the woman’s vagina, and protect the sperm. The vas deferens travel from the testes out of the scrotum and through the lower abdomen via the groin, then around to a point underneath the bladder where they join the urethra. They hold an astonishing amount of sperm: it would take around 30 ejaculations to empty the vas deferens of their full load!
Only around 20 per cent of semen is sperm. The seminal fluid that combines with sperm to form semen is composed of more than 22 different chemicals, including sugar, vitamins C, E and B12, prostaglandins (which help stimulate muscle contractions and the dilatation of blood vessels), the minerals zinc, potassium and sulphur, and essential fatty acids (namely DHA). Altogether, ejaculate consists of around 2 to 4 ml of semen, which is quite viscous at first but then liquefies after about 10 minutes. Sperm need to be nourished by this liquid on their journey, and protected from the acidic environment of the woman’s vagina, before any of them can reach an egg. Around 250 million sperm are ejaculated each time, but it takes only one to fertilize an egg.
Why this enormous quantity of sperm? Only a certain proportion – and this varies from man to man – will be normal, active enough and capable of fertilizing an egg in the first place. Then, because the woman’s vagina is acidic, and hostile to sperm, treating it as it would any other ‘foreign body’ and attempting to get rid of it, as it would an infection, this also reduces the available sperm. From here, only around a million sperm will actually get as far as the woman’s cervix, and only around 200 of these, at most, will reach the woman’s Fallopian tube, to fertilize an egg.
If you then consider how many of the remaining sperm are actually of a good enough quality to fertilize an egg – and in sperm analysis only a maximum of 20 per cent pass this test – it’s no wonder that fertilization can be a tricky business. And even if fertilization does occur, if the sperm responsible is faulty in some way then development of the fertilized egg can’t continue, and miscarriage may be the outcome.
A Good Diet
When you consider what sperm need to develop, and the journey they have to undertake in order to stand a chance of fertilizing an egg, it’s easier to understand why good health in a man is just as important as in a woman when it comes to making babies.
The good news is that, because of the continuous 100-day cycle of sperm production, it is possible to improve sperm’s quality relatively easily, by making the necessary health and lifestyle changes.
While the Nutrition chapter (see page 89) offers general guidelines, it is worth mentioning here, too, that when it comes to the sort of adequate nutrition that makes a difference, there is no point grabbing a general multi – vitamin, or an expensive supplement, unless you know what you’re getting and what you need. Before that, it’s worth looking at your general diet and how to improve it.
Generally speaking, the fresher and less processed the food you eat, the better. Many people advocate organic foods, and there is a good argument for this. In one Danish study, an unexpectedly high sperm count was found among organic farmers. Their sperm count was twice as high as that of a control group of blue – collar workers. But it’s tricky, because if it’s a choice between organic beans flown in from Kenya that have taken five days to get to your supermarket shelf and have then sat in your fridge for two days, and some locally – produced beans that are not organic but were picked yesterday, you might want to choose the latter, as the vitamin and mineral content of the fresher food will be higher, and washing it carefully will help remove chemical and pesticide residues.
Now is not the time to go on some extreme weight – loss diet, either. Some men opt for high – protein diets to lose weight, but we have noticed anecdotally that men following this type of diet have poor sperm. There’s evidence to show that extreme diets, like the low – carb ones in such favour these days, increase the body’s acidity if not actually leaving you malnourished, which won’t be good for sperm production. Better to adjust the balance of what you eat, increase your exercise a little, and reduce your weight that way.
Ideally, you should follow the guidelines set out in the Nutrition and Lifestyle chapters.
Try also to eat a proportion of your foods, especially fresh fruit and vegetables, raw. And when you do cook, try steaming and grilling rather than boiling or frying, which will preserve more of your food’s nutritional value.
It is probably a good idea to cut out all highly processed foods, if you can, as they are alarmingly high in hidden fats, sugars and chemical preservatives. In addition, the nutritional content of food is greatly reduced during processing. Opt for whole foods where you can.
If this feels rather overwhelming, start gradually, introducing a different change into your diet week by week as you adjust.
Water
When it comes to what you drink (and alcohol is covered separately: see page 62), make sure you are not over – doing your caffeine intake. Caffeine is mildly addictive, so if you are used to drinking a lot it may take a while to kick the habit. There is also some evidence to show that if a man has a high caffeine intake before conception, the risk of premature birth is increased. Tea contains tannin, which is less of a stimulant than caffeine, but excess quantities will deplete you of iron.
Most men do not drink enough water. Sperm need to swim!
Start changing your drinking habits first of all by increasing your water intake – most of us drink too little, generally, to be adequately hydrated.
What Do Sperm Need?
There is a lot of research available now about free radical damage to sperm, but thankfully there’s a lot you can do to improve this. To produce sperm your body needs a good intake of certain nutrients, which may need supplementing if they are not readily available from your diet. Research has shown that certain vitamins and minerals improve overall sperm counts – I’ve seen it many times. It is important, however, to remember not to exceed the recommended daily allowance (RDA) of any one item, even if you have heard that it might be beneficial, unless under supervision from a health professional. An excess of one item can deplete others, so a balance is needed.
Also see the Nutrition chapter for more advice on how to improve your diet to increase the chances of conception.
Vitamin C
A well – known antioxidant, under normal conditions vitamin C protects sperm from oxidative damage, and certainly improves sperm quality in men who smoke. However, some men have a condition of their sperm called ‘agglutination’ where sperm clump together and fertility is reduced. In these cases, vitamin C supplementation of up to 1 gram a day helps reduce agglutination – and was shown to increase fertility in one group of men in a controlled study.
Zinc
Semen is rich in zinc, and men lose a certain amount of this mineral per ejaculate. Zinc is often referred to as the ‘fertility mineral’ and its presence in foods like oysters, which are said to have aphrodisiac properties, may reinforce this idea! Certainly an insufficiency of zinc can lead to both reduced numbers of sperm and impotence in some men. It has also been found that the levels of zinc in the semen of infertile men are of a lower level than in fertile men. Numerous studies have been done, and some of the results seem to conflict, but overall there is enough evidence to suggest that for men with poor sperm quality, sperm count and sperm motility, a supplement of zinc can help.
In areas of the country where the copper content of water is naturally high there may be a general zinc deficiency, as these two minerals have to be in balance: an excess of copper can reduce zinc. Conversely, where long – term zinc supplementation is recommended, then supplementation with copper is needed.
Vitamin B12
Necessary to maintain fertility, there are studies that have shown an improvement in sperm motility where oral vitamin B12 was given. In the latter case, around 60 per cent of those men who received an oral supplement of vitamin B12 (1,500 mcg per day of methylcobalamin) had improved sperm counts.
Vitamin E
Certainly a deficiency in vitamin E, in animals, leads to infertility. In one human trial, the giving of 100–200 iu of vitamin E daily to both partners led to a significant increase in fertility. Vitamin E seems to reduce the amount of free – radical damage done to cells. Supplementing reduces the amount of oxidative stress on sperm cells, although it should be said that the research is at a preliminary stage and needs further work before a definite case for sperm improvement can be made.
Co-enzyme Q10
This is a nutrient used by the body’s cells in the production of energy. Its exact role in the production of sperm isn’t known, but there is evidence to show that as little as 10mg a day over a two – week period will improve both sperm count and motility. In one study, where men with low sperm counts were given 60mg a day over a three – month period, although no significant change was observed in most measures of sperm quality and quantity, in – vitro fertilization rates improved significantly.
Selenium
This is an essential trace mineral that acts with the antioxidant vitamins A, C and E, and is found in large quantities in Brazil nuts. In one double – blind study of infertile men, supplementation of 100 mcg per day of selenium for three months significantly increased sperm motility, but not sperm count.
Calcium
The motility of sperm is partly determined by the concentration of calcium in semen, and this mineral is also a key regulator of human sperm function. However, although we know it is important there has been no evidence to confirm that a calcium deficiency causes male infertility. Neither is there any evidence to show that calcium supplementation improves male infertility.
Pycnogenol
Pycnogenol (French maritime pine bark extract) is a natural antioxidant that has been found useful in maintaining the health of blood vessel walls and circulation. It works, at least in part, by subduing free radicals. A preliminary study recently presented at the 54th Annual Meeting of the American Society for Reproductive Medicine/16th World Congress on Fertility and Sterility in San Francisco reported the findings of Dr Scott J. Roseff and his colleagues at the West Essex Center for Advanced Reproductive Endocrinology in West Orange, New Jersey. In the study, four ‘subfertile’ male patients took daily supplements of Pycnogenol® for three months. These men had had relatively high numbers of deformed sperm, as well as low sperm counts and activity. After 90 days, the percentage of structurally normal sperm – that is, non – deformed sperm – increased by an average of 99 per cent. ‘The number of deformed sperm went down and the number of normal sperm went up,’ Dr Roseff said. ‘The increase in morphologically (structurally) normal sperm is significant, although this is just a preliminary study. Pycnogenol could enable some couples to forego expensive in – vitro fertilization in favour of simpler and less expensive intrauterine insemination.’