Полная версия
Pediatric stroke. Revascularization and reconstructive surgery in children with cerebrovascular disease

Pediatric stroke
Revascularization and reconstructive surgery in children with cerebrovascular disease
Authors: Shevchenko E. V., Usachev D. Y., Belousova O. B., Lukshin V. A., Lvova O. A.
© E. V. Shevchenko, 2019
© D. Y. Usachev, 2019
© O. B. Belousova, 2019
© V. A. Lukshin, 2019
© O. A. Lvova, 2019
ISBN 978-5-4493-4265-2
Created with Ridero smart publishing system
Writing Team
Olga Benuanovna Belousova
Neurologist, Dr. Med. Sci., leading research scientist in the Clinical Vascular Neurosurgery Department of FSAI «Burdenko Neurosurgery Institute» of the Ministry of Healthcare of the Russian Federation
Anton Evgenyevich Korshunov
Neurosurgeon, Cand. Med. Sci., senior research scientist in the Clinical Pediatric Department of FSAI «Burdenko Neurosurgery Institute» of the Ministry of Healthcare of the Russian Federation
Irina Andreyevna Nagorskaya
Medical Psychologist, Cand. Psych. Sci., Medical Psychologist in the Mental Research Team of FSAI «Burdenko Neurosurgery Institute» of the Ministry of Healthcare of the Russian Federation
Vasiliy Andreyevich Lukshin
Neurosurgeon, Cand. Med. Sci., senior research scientist in the Clinical Vascular Neurosurgery Department of FSAI «Burdenko Neurosurgery Institute» of the Ministry of Healthcare of the Russian Federation
Olga Aleksandrovna Lvova
Pediatric Neurologist, Dr. Med. Sci., assistant professor in Chair of Psychiatry, FSBEI of Higher Professional Education «Urals State Medical University» of the Ministry of Healthcare of the Russian Federation, leading research scientist in the Laboratory of Brain and Neurocognitive Development of FSAEI of Higher Professional Education «Ural Federal University named after the first President of Russia B.N. Yeltsin»
Olga Borisovna Sazonova
Neurophysiologist, Cand. Med. Sci., leading research scientist in the Laboratory of Clinical Neurophysiology of FSAI «Burdenko Neurosurgery Institute» of the Ministry of Healthcare of the Russian Federation
Elena Viktorovna Shevchenko
Neurosurgeon, Cand. Med. Sci., junior research scientist in the Clinical Vascular Neurosurgery Department of FSAI «Burdenko Neurosurgery Institute» of the Ministry of Healthcare of the Russian Federation
Lyudmila Valentinovna Shishkina
Pathomorphologist, Cand. Med. Sci., Head of Laboratory of Pathomorphology in FSAI «Burdenko Neurosurgery Institute» of the Ministry of Healthcare of the Russian Federation
Dmitry Yuryevich Usachev
Neurosurgeon, Corresponding Member of the Russian Academy of Sciences, Dr. Med. Sci.,Prof., Deputy Director for Science of FSAI «Burdenko Neurosurgery Institute» of the Ministry of Healthcare of the Russian Federation
List of acronyms and conventional symbols
ABP – arterial blood pressureACA – anterior cerebral arteryACVD – acute cerebrovascular diseaseADHD – attention deficiency and hyperactivitydisorderADP test – adenosine diphosphate inducedplatelet aggregation testAHT – arterial hypertensionASA – acetylsalicylic acidASL – Arterial Spin LabeledASPI test – arachidonic acid inducedplatelet aggregation testBCA – brachiocephalic arteriesCAG – cerebral angiographyCCA – common carotid arteryCCVD – complete cerebrovascular disease /complete strokeCN – cerebral nervesCNS – central nervous systemCO – cerebral oximetryCPISR – Canadian Pediatric Ischemic Stroke RegistryCVD – cerebrovascular diseaseCVS – cardiovascular systemDEP – dyscirculatory encephalopathyDMB – dura mater of brainECA – external carotid arteryECG – electrocardiographyEchoCG – echo-cardiographyEDAS – encephalo-duro-arterio-synangiosisEDMS – encephalo-duro-myo-synangiosisEEG – electro-encephalographyEICMA – extra-intracranial microvascularanastomosisEMS – encephalo-myo-synangiosisICA – internal carotid arteryINR – international normalized ratioIS (AIS) – ischemic stroke (arterial ischemic stroke)LBFR – linear blood flow rateMASGS – Modified Ashworth Scale ofGrading SpasticityMCA – middle cerebral arteryMONICA – The World Health Organization’sMultinational Monitoring of Trends andDeterminants in Cardiovascular DiseaseMRA – magnetic resonance angiographyMRI – magnetic resonance imagingNIHSS – National Institutes of Health Stroke ScaleNSA – National Stroke AssociationOA – occipital arteryPCA – posterior cerebral arteryPComA – posterior communicating arteryPET – positron emission tomographyPS – pial synangiosisSCT AG – spiral computed angiographySCT or CT – spiral computer tomographySTA – superficial temporal arteryTCUSDG – transcranial ultrasonic dopplerographyTIA – transitory ischemic attacksUS – ultrasonographyVBS – vertebrobasilar systemWHO – World Health OrganizationIntroduction
Pediatric stroke. Revascularization and
reconstructive surgery in children
Pediatric stroke is one of the most widely discussed problems in contemporary medicine. This is, primarily, associated with the fact that a cerebral vascular disease (CVD) is considerably less common in childhood than in adults, and, therefore, less known. At the same time, children, who had suffered CVD, constitute an essential group among disabled children. This determines the need for a closer study of the pediatric stroke problem, particularly, in the background of successful conservative and surgical treatment of strokes in adult population.
The spectrum of clinical manifestations of the pediatric stroke is wide enough – from mild focal and isolated general cerebral symptoms to the formation of a significant neurologic deficiency with a predisposition to recurrence with the subsequent sustained disability and a high risk of fatality. Thanks to a widespread distribution and technical improvement of neuroimaging methods, the pediatric stroke is diagnosed with the ever increasing frequency. Nevertheless, the low awareness of neurologists about the CVD problem in childhood, including the transitory ischemic attacks (TIAs), frequently leads to difficulties in diagnostics and, consequently, to delayed and insufficient medical aid. Due to the variety of reasons, clinical manifestations and the course of the pediatric stroke, selecting the patient management approach becomes difficult, especially, in neurology and brain surgery departments in small city hospitals, where medical specialists lack sufficient experience in treatment of this disease.
This book presents basic literature data on etiology, pathogenesis, clinical manifestations of a pediatric stroke, examination methods and approach to the conservative and surgical treatment of acute and chronic cerebral ischemia in children as well as our own studies on diagnostics and results of conservative and surgical treatment of children with the disease onset at the age of the 1-st day of life up to 18 years old, all obtained on the basis of Burdenko Neurosurgery Institute and FSBEI of Higher Professional Education «Urals State Medical University» of the Ministry of Healthcare of the Russian Federation.
This book will enable a wide range of pediatric specialists to get an idea about the specific features of a pediatric ischemic stroke, its diagnostics, conservative treatment principles and options for surgical treatment of this disease.
Chapter I.
Pediatric stroke. General information
Nowadays, the mortality rate of cerebrovascular diseases in Russia is one of the world’s highest. A cerebrovascular disease holds one of the first places among the most frequent mortality and disability causes, just as in economically developed countries too. The World Health Organization’s Multinational Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA) determines the course of a stroke as «a sudden neurologic deficiency sustaining for over 24 hours, or a sudden death». This definition includes both ischemic and hemorrhagic strokes [262].
In a pediatric population, an ischemic stroke is a less frequent pathology as compared to the adult population. Strokes occur in children of any age [33]. Delayed or erroneous diagnosis of a stroke in children still remains a common enough event [80; 104].
The descriptions of individual clinical cases of cerebrovascular diseases in children can be found in literature since the 17-th century. The first description of a stroke in a child is considered to be made by T. Willis in 1667. J. Wepfer (1658) mentioned sick children, who had a hemiplegia, which was emerging and regressing within a day or faster [278]. The disease termed as «an infantile hemiplegia» was presented in the works by W. Osler (1889), B. Sachs and F. Peterson (1890) as well as S. Freud (1893) in a series of pediatric patients, who had suffered a stroke. It was only in 1927 that F. Ford and A. Schaffer published the first ever systematized description of methods for assessment and treatment of children with ischemic strokes. The authors analyzed the etiology of a pediatric stroke as well as the methods and the results of treatment, which had a subsequent effect on the quality of life [98]. V. Hachinski (1982) described non-specific symptoms, such as a headache and syncopes [118]. It is important to note that many problems outlined by them still remain pertinent even today.
The works by M. Norman (1957), C. Fischer (1959), E. Frantzen (1961), E. Bickertaff (1964), J. Jackson (1970), J. Abraham (1971), W. Kannel (1972) about pediatric strokes are, doubtless, interesting, although these publications did not contain any mentioning of the transient cerebrovascular diseases in childhood [131]. In later studies, the transient cerebrovascular diseases, or, in other terms, the transitory ischemic attacks (TIAs), were noted to occur in children much more frequently than strokes [209]. In 2006 G. Ganesan et al. published an article on the results of a retrospective (from 1978 to 1990) and prospective (from 1990 to 2000) survey of children, who had suffered a stroke, with the use of a neuroimaging. They described 212 patients, including 97 ones with an erroneous initial diagnosis. 79 children were noted to have a growing neurologic deficiency (29 strokes, 46 TIAs, 4 fatal cases due to a recurrent stroke), while during the analysis of the subsequent 5 years 51 children (67%) were noted to have recurrent episodes of cerebrovascular diseases [104].
The number of publications on the subject of a pediatric stroke is growing worldwide with every year. In recent years, educational seminars and topical sessions on this problem appeared in the European Stroke Organization Congress program (Nice, 2014; Glasgow, 2015; Barcelona, 2016). Nowadays, practitioners working abroad can be guided by two manuals: an American one – «Management of Stroke in Infants and Children» released in 2008 and a European one – «Stroke and cerebrovascular disease in childhood» published in 2011 in London [105; 267]. Thus, practical manuals accumulating the results of scientific research and permitting to make clinical decisions are solitary and rarely updated.
The lack of universally accepted international recommendations or guidelines hampers the choice of approaches to treatment and prevention of pediatric strokes. A low awareness of pediatric neurologists on the problem of pediatric strokes and TIAs often leads to difficulties in diagnostics and inadequate therapy of pediatric patients and, therefore, to a delayed and inadequate care, which was noted by V.P. Zykov (2008), F. Kirkham (2011) and A. Mallick (2014) in their works. The main drawback of the research studies presented in literature consists in the fact that only some individual states were specified as those relevant to risks, which, as a rule, was determined by the specialty of a research team (infectologists, rheumatologists, geneticists, hematologists, etc.). The paucity of assessed sampling children in these studies and the restriction of data acquisition to a specific age group (infants, teenagers, etc.) hampered the potential generalization of results obtained within the boundaries of all age groups.
1. Epidemiology
The rate of strokes in the adult population of the Russian Federation is about 500,000 cases per annum, the average stroke morbidity rate is 4.6 incidents per 1,000 of the population annually (the NSA data, 2003).
According to literature data, the average global pediatric stroke morbidity rate varies within a range of 0.93 – 13 incidents per 100,000 of the population annually [33]. According to data of the American Heart Association & American Stroke Association, 2012, the highest stroke incidence rate is noted during the first year of life – approximately 1 incident per 4,000 liveborns [219]. The stroke morbidity rate in children aged from 0 to 15 years in the USA is 6.4 incidents per 100,000 children [222]. During the last 10 years, this number remained stable, but the recent research showed that the incidence rate was 3—4 times higher, than it had been stated earlier [39].
M. Giroud et al. (France, 1995) report that in children below 16 years old the CVD incidence rate reaches 13 incidents per 100,000 children annually. This number includes 7.9 cases of ischemic CVD per 100,000 children and 5.1 cases of hemorrhagic CVD [110].
According to data of the Canadian Pediatric Ischemic Stroke Registry (CPISR), in 2000 this parameter was recorded at the level of 2.7 incidents per 100,000 annually [160]. F. Kirkham et al. reported that in 2004 the incidence rate of CVD in British children was 13 incidents per 100,000 of pediatric population [143].
Thus, according to various data, the morbidity rate of pediatric hemorrhagic stroke at the age from 1 month to 18 years varies from 1.5 to 5.1 (on the average, 2.9) and that of the ischemic stroke – from 0.6 to 7.9 incidents per 100,000 of the population annually. Also, there are some data on the percentage ratio of these two types of strokes: 55% is accounted for ischemic strokes and 45% – for hemorrhagic ones [77]. At the same time, in newborns this parameter is considerably higher for both types of CVD: 6.7 and 17.8 per 100,000 of the population annually for hemorrhagic and ischemic types of CVD respectively [11; 167; 215].
These figures show that, generally, the ischemic stroke incidence rate in children is higher than the hemorrhagic one, although this difference is not as big as in adults [8; 33; 40], which makes the CVD structure in children essentially different.
During the period from 1979 till 1998, in the USA the child mortality decreased by 58%. Such a decrease is deemed to occur due to the improvement of the treatment quality, not due to the drop in stroke morbidity rate [149]. According to latest data, from 20% to 40% of children die after the strokes in the USA [219], and the stroke is among ten leading causes of child mortality [68]; about 3,000 children and teenagers (below 18 years old) suffered a stroke in 2004 [149]; during the period from birth to an age of 18 years old the stroke risk is almost 11 incidents per 100,000 children annually [219]; strokes occur in boys approximately 1.3 times more frequently than in girls [222]; in Afro-American children the stroke risk is higher than in children from Europe and Asia [222].
The stroke mortality in children varies from 7% to 28% [100; 161], being higher in hemorrhagic strokes (up to 40%) than in ischemic ones (8—16%). The fatal outcome usually occurs in the early rehabilitation period, which is deemed to be the most dangerous time for recurring acute vascular episodes and patient death. Such indicators in children with ACVD are, generally, consistent with the statistical data on adults. However, the mortality level of 10%-40% may be regarded as the highest-ever for pediatric practice, which permits to determine strokes in this age group as one of the emergency pathologies threatening with fatal impairment of vital functions.
The official statistics on pediatric stroke morbidity rate in our country are not available [33]. In literature there are some data for individual areas or institutions. Specifically, based on an example with one of the central regions of Russia, V.M. Delyagin et al. (FSI «Federal Research & Clinical Centre of Pediatric Hematology, Oncology and Immunology», Moscow) reported that during the period from 2006 to 2009 the ACVD morbidity rate among children (excluding newborns) was from 0.93 to 1.1 incidents per 100,000 children annually. When estimating the number of children and teenagers with strokes per total number of children taken to multidisciplinary children’s hospitals, the stroke incidence rate is 3.5 per 1,000 patients annually [7; 11], which corresponds to data of foreign multi-center surveys. This number includes 2.8 children aged from 0 to 11 years old per 1,000 patients annually and 0.7 children aged from 12 to 17 years old (teenagers) per 1,000 annually; the average pediatric stroke morbidity rate (from 1 month to 18 years old) is about 8 incidents per 100,000 of population annually. The mortality among children with CVD reaches 0.6 per 100,000 of population annually [8].
Having analyzed the data on 143 patients aged from 0 to 17 years old with CVD (the age median of 5 years old, in 68 boys (48%) and 75 girls (52%)), the same authors concluded that all types of CVD occur equally often both in boys and girls, with the exception of TIAs, which are recorded in girls three times more frequently than in boys. The authors also note a high percentage (13%) of recurrent strokes in children, while the highest risk of a recurrent CVD is recorded during the first 2 weeks after the disease onset [8].
According to data of the Emergency Call Service of Moscow, in 2012 there were 157 ambulance responses on calls to children and teenagers with the ACVD diagnosis, and in 2013 – 179 [4].
Employees of the FSBEI of Higher Professional Education «Urals State Medical University» analyzed the stroke in children living in the area of Yekaterinburg (with population of 1.5 million people) and Sverdlovsk region (4.5 million people). The following parameters were assessed: the stroke registration rate in the years from 1995 till 2015; the morbidity rate during the last five years, including children of the first year of life; gender distribution characteristics; incidence rate of fatal outcomes and recurrences in 162 children with IS and 73 children with TIA.
The study was held for 10 years. During this period, the information was distributed among the pediatric neurologists of the city and the region, who actively referred already followed-up and new pediatric patients with diagnosed or suspected ischemic ACVD to hospitals. We suppose that practically all patients with the onset of IS or TIA occurring in childhood were included into this database, and this permits to regard this study as an epidemiological survey.
According to the data obtained, during the last five years the morbidity rate was: 3.4 (2011), 4.9 (2012), 4.9 (2013), 4.6 (2014) and 5.0 (2015) per 100,000 of the pediatric population annually. Fig. 1 shows the total number of registered children with strokes on a specified territory during the last 20 years since 1995, when neuroimaging (brain CT) and emergency diagnosing became possible.
It must be emphasized that the obtained indicators are closer to the lower threshold of values stated in literature (2—26.7 per 100,000 annually). At the same time, a distinct tendency for growing stroke registration incidence rate in children in the surveyed area, which can be observed during the last ten year period in all countries, where ACVD morbidity is registered among children.
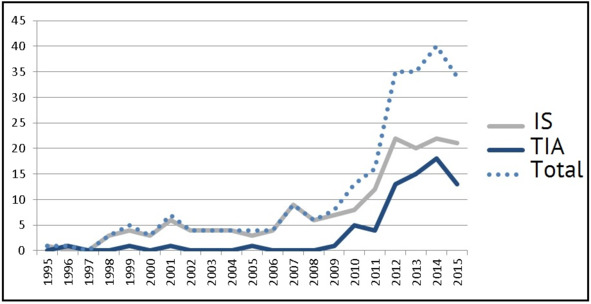
Fig. 1. Incidence rate of ischemic stroke in children in 1995—2015 in the area of Yekaterinburg and Sverdlovsk region (population: 6 million people).
The average age of children with IS manifestation at the age of below one year was 19.5±1.2 weeks (we revealed 7 infants with fetal / perinatal onset of IS) and at the age of above one year – 6.2±0.4 years. For TIA this parameter was 11.8±0.3 years.
The gender distribution of patients was even, and matched the literature data: boys with IS constituted 62.7% (n=102), and boys with TIA – 45.2% (n=33).
Based on literature data, the average risk of recurrent strokes in children is 20%, while in children with a single revealed risk this parameter is within 8%, and in children with a combination of two or more risks it grows at an exponential rate and reaches 42% [145; 148].
According to data of the FSBEI of Higher Professional Education «Urals State Medical University», the recurrence is also recorded on the levels of 14.2% (n=23) and 70.4% (n=50) for IS and TIA respectively. The average incidence rate of recurrent ISs was 1.6±1.1 (1—2 episodes of IS compared to 2—19 incidents of TIA), the average incidence rate of TIA was 3.4±0.5 incidents (from 2 to 20 episodes). It is the low level of ACVD detectability in childhood, which is supposed to cause the lack of timely and comprehensive examination, correct diagnosing and timely application of secondary prevention measures. For example, there was a patient registered, who had suffered 6 TIAs and 2 ISs, before he was subjected to a comprehensive examination, which diagnosed the moya-moya disease.
The disability status was given to 61.2% (n=90) and 9.1% (n=4) of patients from 125 and 62 children with IS and TIAs respectively, whose catamnesis was known. It should be noted that the disability in the group of children with TIAs was caused by a non-neurologic deficiency: two children had an acknowledged moya-moya disease, one had a chronic renal insufficiency, and one – a congenital heart defect.
The mortality in a group of children with IS was 3.3% (n=4, 2 boys and 2 girls); all the patients, who had suffered TIAs, were alive by the moment of the last follow-up visit (minimum 2 years of follow-up).
Thus, the literature data and the results of limited epidemiological surveys in Russia permit to conclude that ischemic strokes are a relatively rare disease in pediatric practice, although they are characterized by a high rate of recurrence, disability and mortality.
2. Pediatric stroke classifications
As already stated above, the ratio between hemorrhagic and ischemic strokes in children essentially differs from that in an adult age group. There is no unanimous opinion on the ratio between these variants in children. Apparently, the prevalence of an ischemic or a hemorrhagic ACVD variant in every new survey is associated with the specialization profile and medical care type in a healthcare facility.
Also, there are discrepancies in determination of a stroke variant in a child. For instance, the national research community failed to agree whether periventricular ischemia as well as intraventricular and subarachnoid hemorrhages can, by way of a morphological substrate of perinatal impairment of infants’ nervous systems, be considered to be equivalents of ischemic or hemorrhagic ACVDs (by analogy with adult patients). Authors of foreign clinical manuals on diagnostics and treatment of strokes say that they excluded infants with such lesions from analyzed literature sources. Based on provided epidemiological indicators, it also becomes evident that the researchers did not include patients with perinatal encephalopathy into their analysis scope [183; 107; 146; 220; 280].

