
Полная версия
Anatomy of bone system. The manual for medical students / Анатомия костной системы. Учебное пособие для медицинских вузов
The proportion of organic and inorganic substances in bones primarily depends on age, and it may change under the influence of various reasons (climatic conditions, nutrition, diseases). Thus in children, bones contain much less mineral (inorganic) substances, therefore they are more flexible and less solid. In elderly persons, vise versa, the amount of organic substances decreases. In such age, bones become more fragile and susceptible to fractures.
1.6. Mechanical Properties of Bones
The bone is a solid object, and its main properties are durability and elasticity. Durability is the ability to resist to the external destroying force. It depends on the macro- and microscopic structure, and on the osseous tissue composition. As for the macroscopic structure, each bone has its specific form which enables withstanding the maximal strain in a certain part of the skeleton.
The internal structure of the bone is also complicated. As already stated, the osteon is a hollow cylinder tube the walls of which are built of numerous lamellae. It is known that in architectural constructions, hollow (tubular) columns have greater durability per a unit of mass as compared to solid columns. Therefore, the osteon-based structure of the bone itself predetermines a high level of its durability. Groups of osteal lamellae, being arranged along the axes of maximal strains, form osteal trabeculae of spongy bone and terminal lamellae of compact bone. It should be noted that osteal trabeculae are archshaped in places of maximal strains. As well as tubular systems, arch-shaped systems are most durable. The arch principle in the structure of spongy bone trabeculae is typical of the proximal epiphysis of the femur, as well as of the calcaneus spongy tissue etc.
The bone composition significantly influences its durability. Decalcification causes a considerable decrease in the level of compression, tension and torsion strength. As a result, it is easy to bend, compress and twist the bone. If the calcium content increases, the bone becomes fragile.
Bone durability in a healthy adult is higher than the durability of some construction materials – it is like a cast iron. The first examinations of bone durability were conducted in XIX century. According to Lesgaft`s researches, the human bone withstood tensile strain of 5500 N/cm2, compressive strain – 7787 N/cm2. The tibia withstood compressive strain of 1650 N/cm2, whichis comparable to the weight of more than 20 men. These data show a high level of reserve capabilities of bones against various strains. Changes in the tubular structure of a bone (both macro- and microscopic) reduces its mechanical durability. For example, the tubular structure of bones is disrupted after fracture healing, and the durability of such bones significantly decreases.
Elasticity is the ability to regain the initial shape after cessation of an external impact. Bone elasticity is equal to that of hard tree species. Like durability, it depends on the macro- and misroscopic structure and the chemical composition of the bone.
Thus, the mechanical properties of bones – durability and elasticity – are predetermined by the optimal combination of organic and inorganic substances contained in them.
1.7. Functions of Skeleton
1. The bones serve as support for soft tissues (muscles, ligaments, fasciae, visceral organs).
2. Most of bones are leverages which are moved by attached muscles. According to these two functions, the skeleton may be considered to be the passive part of the musculoskeletal system.
3. The human skeleton is an antigravitational structure which counteracts the force of gravity. It prevents any changes in the body shape under the impact of gravitation pressing the human body to the ground.
4. Protective function: the skull, trunk and pelvis bones prevent any potential damage to the vital organs, major vessels and nerve trunks. For example, the skull encloses the brain, organs of vision, hearing and equilibrium. In the vertebral canal there is the spinal cord. The chest protects the heart, lungs, major vessels and nerve trunks. The pelvic bones protect the rectum, urinary bladder and internal genital organs against injuries.
5. Hematopoietic function: most bones contain red bone marrow which is the hematopoietic organ, as well asthe immune system organ. The bones protect the red bone marrow against damages, and provide favorable conditions for its trophism and for maturation of blood elements.
6. Involvement in mineral metabolism: bones deposit numerous chemical elements, predominantly calcium and phosphorus salts.
According to V. S. Speransky, the human skeleton is a perfect dynamic structure adapted to the motor function and human way of life; it is responsive to various changes which occur both in the body itself and in the environment.
1.8. Development of Bones
The osseous tissue appears in the human embryo in the middle of the second month of fetal development, when all other tissues have been already formed. The development of bones may proceed in two ways: on the basis of connective tissue and on the basis of cartilage. It should be noted that connective tissue never turns directly into cartilaginous tissue or osseous tissue. Osseous tissue is capable of developing by the way of growth along the surface of connective tissue or cartilage (appositional bone growth), or it develops to replace a resorbed cartilage.
Bones developing on the basis of connective tissue are termed primary. They are calvarial bones, and viscerocranial bones. Ossification of the primary bones is termed endesmal. It occurs in the following way: within the anlage of connective tissue, an ossification centre, punctum ossificationis (centrum ossificationis), appears and then expands into the depth and across the surface. From the ossification centre, osteal trabeculae start to form along the radii. They are interconnected with bone rods. In these spaces between the rods there are red bone marrow and blood vessels. In most of primary (membrane) bones, not one but several ossification centres are formed. They gradually grow and merge with each other. Eventually, only the most superficial layer of the initial connective tissue stratum remains unchanged. Then this layer turns into the periosteum.
Bones developing on the basis of cartilages are termed secondary. They pass through connective, cartilaginous and, in the last turn, osseous stages. Secondary bones are the skull base bones, trunk bones and bones of extremities. Let`s study the development of a secondary bone on the example of the long tubular bone. By the end of the second month of the fetal period, the cartilaginous anlage appears; it resembles a definite bone by shape. The cartilaginous anlage is covered by perichondrium. In the area of the future diaphysis of the bone, the perichondrium transforms into the periosteum. Lime salts are accumulated in the cartilaginous tissue under the periosteum, and cartilaginous cells die away. The osteal cells – osteoblasts – come from the periosteum to replace the dead cells. They start to produce an organic matrix of osseous tissue which endures calcification. The osteoblasts enclosed in the intercellular substance transform into osteosytes. Thus, the osteal cylinder termed periosteal or perichondral bone is formed in the diaphysis area. This stage of ossification of secondary bones is termed perichondral. Subsequently, new bone layers overgrow from the periosteum. Bone lamellae evolve, i.e. Haversian systems (osteons) start to develop around the vessels growing from the periosteum. The vessels sprouting from the periosteum are directed to the midst of the cartilaginous anlage. The cartilage located in the center of the diaphysis accumulates lime salts, dissolves and is substituted by spongy bone. This process is termed enchondral ossification of the diaphysis. The medullary canal is absent at first. It is formed in the process of transformation of spongy tissue of the enchondral bone inside the diaphysis and during red bone marrow development inside it.
In the epiphyses, ossification starts later, some bones are ossified even after the birth. Ossification begins from the ossification centre which appears within the cartilaginous anlage of the epiphysis. Such ossification process is called enchondral. It occurs in the following way: firstly, from the periosteum, blood vessels sprout into depth of the cartilage along the radii. In the midst of the epiphysis, the cartilage accumulates lime salts, dissolves and is substituted by osseous tissue. Later, the periosteal (perichondral) bone develops from the periosteum along the edge of the cartilaginous anlage of the epiphysis. The periosteal bone is comprised by a thin layer of compact tissue. The perichondral lamina is absent only in the areas of future articular surfaces – a quite thick layer of cartilage remains there. The cartilaginous layer also remains between the epiphysis and diaphysis – this is a metaepiphysial cartilage. It is the area of bone growth in length, and it disappears (transforms into osseous tissue) only after bone growth stops.
In long tubular bones, individual ossification centres appear in each epiphysis. Fusion of the epiphyses with the diaphysis usually occurs after birth. For example, in the tibia, the lower epiphysis merges with the diaphysis by the age of about 22 years, and the upper epiphysis – by 24 years. Short tubular bones normally have the ossification centre only in one epiphysis, the other epiphysis is ossified from the diaphysis. Some tubular bones have several ossification centres in their epiphysis at the same time. For example, in the upper epiphysis of the humerus, three centers appear; in the lower epiphysis of the humerus – there are four centers.
Volumetric bones are ossified like the epiphyses of long tubular bones i.e. enchondral ossification precedes periostal ossification. In flat bones, this process occurs vice versa, i.e. periostal ossification precedes ehchondral ossification.
It should be noted that, besides the main ossification centres, additional ossification centres may exist. They appear much later than the main centres. With the coming puberty, metaepiphysial cartilages become thinner and are replaced with osseous tissue. In the skeleton, synostoses start to develop. The distal epiphysis of the humerus and the epiphyses of the metacarpals are the first to fuse with their diaphyses. Formation of the synostoses comes to an end by about 24–25 years. Bone growth terminates when all the main and additional centers merge into one solid mass, i.e. when the cartilaginous layers separating the bone parts from each other disappear.
Significant individual differences in ossification rates are observed. The process of skeleton ossification in a child may be accelerated or decelerated; it depends on the genetic, hormonal and environmental factors. The term «osteal age» is used to assess the process of skeleton development in children. It is determined according to the number of ossification centres in bones and according to the time of their fusion. To evaluate ossification, roentgenography of the hand is made, because the age dynamics of ossification centre appearance and formation of synostosis are very clearly manifested in this part of the body. Ossification centres in carpal bones appear in the following periods:
– at birth, carpal bones are cartilaginous;
– ossification points emerge in the capitate and hamate bones during the first year of life;
– in the triquetral bone – during the third year of life;
– in the lunate bone – during the fourth year of life;
– in the scaphoid bone – during the fifth year of life;
– in the trapezium and trapezoid bones – during the sixth-seventh years of life;
– in the pisiform bone – in the tenth-fourteenth years of life.
Ossifcation of free parts of limbs is given in fig. 1.5.
V.S. Speransky distinguishes the following characteristic features in the ossification process:
1) ossification starts earlier in the connective tissue than in the cartilage;
2) ossification of the skeleton occurs in the cranial-caudal direction;
3) skull ossification spreads from the viscerocranium to the neurocranium;
4) in the free parts of extremities, ossification occurs from the proximal regions to the distal areas.
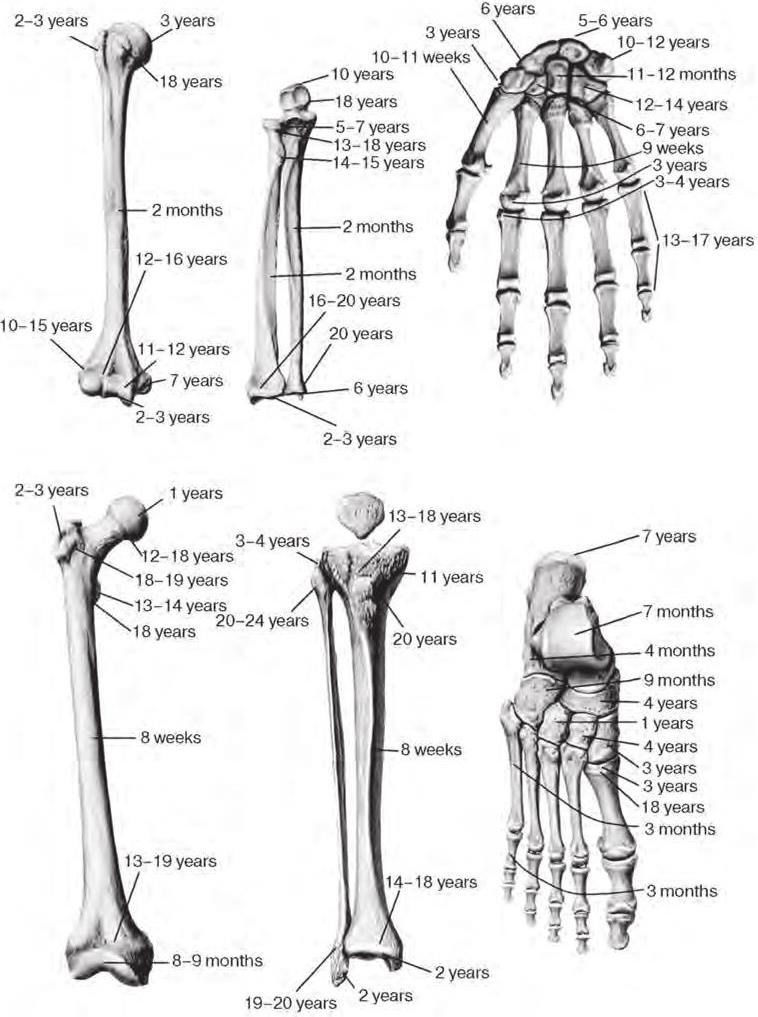
Fig. 1.5. Periods of ossification of free parts of limbs in male (Alexina L.A., 1985, 1998)
Osteal age does not always coincide with the passport age. In some children, the ossification process terminates 1–2 years earlier than it happens normally, in others – 1–2 years later. Starting from the age of 9 years, sexual differences of ossification can be distinguished clearly – in girls this process occurs more rapidly.
Body growth in girls terminates mainly at the age of about 16–17 years, in boys – at about 17–18 years. After this age, body growth in length is no more than 2 %.
In old age, bone rarefication termed osteoporosis occurs in different parts of the skeleton. In tubular bones, osseous tissue dissolves inside the diaphysis, as a result, the medullary cavity becomes wider.
At the same time, calcium salts are accumulated, and osseous tissue is developed on the outer surface of the bone, under the periosteum. Quite often, in places of attachment of ligaments and tendons, bony outgrowths called osteophytes develop. They also emerge along the edges of articular surfaces. In elderly persons, bone durability considerably decreases, and even minor injuries may cause fractures.
Skeleton ageing is characterized by individual changeability. In some persons, ageing symptoms appear as early as at the age of 35–40 years, in other persons – only after 70. Skeleton ageing symptoms are more manifested in women than in men. But this process significantly depends on the complex of factors: genetic, climatic, hormonal, alimentary (nutritive), functional, ecological etc.
1.9. Anomalies of Bone Development
1. Osteomalacia – disorder of calcification of newly formed osseous tissue which is caused by deficiency in calcium or vitamin D.
2. Osteoporosis – disorder of formation of the bony matrix during the skeleton formation (insufficient compensation of resorbed bone tissue). It occurs in elderly and old age and is caused by exessive resorption of osseous tissue.
3. Ectopic osteogenesis – ossification of soft tissues in abnormal places (in walls of arteries, kidneys etc.)
TEST QUESTIONS
1. What function does the skeleton carry out?
2. Name the types and functions of the bone marrow.
3. List the principles of the bone classification.
4. Give the characteristic of the primary and secondary bones.
5. What organic and inorganic substances are included into the composition of the bone (in what ratio)?
6. What connective tissue structure covers the bone from outside? What is its function?
7. What is the structural unit of osseous tissue? Name the types of osteocytes.
CLINICOANATOMICAL PROBLEM
During the surgical operation in a 10-year-old patient the metaepiphysial cartilage which separates the head of humerus from the body of humerus, was radically removed. What is the prognosis?
2. SKELETON OF TRUNK
The skeleton of trunk consists of the vertebral column, or backbone, columna vertebralis, and the thorax, cavea thoracis (thorax).
The vertebral column in an adult person consists of 24 individual vertebrae, sacrum and coccyx. There are the cervical vertebrae (7), thoracic (12) and lumbar ones (5) distinguished in the vertebral column. The sacrum consists of five fused sacral vertebrae. The coccyx consists of 3–5 fused coccygeal vertebrae. The thorax consists of 12 pairs of ribs with corresponding thoracic vertebrae and the sternum.
2.1. General Vertebral Features
The vertebra, vertebra, is comprised of the vertebral body, corpus vertebrae, anteriorly, the vertebral arch, arcus vertebrae, posteriorly and vertebral processes, processus vertebrae. The vertebral body is anterior and supporting part of the vertebra. The arch is located behind the vertebral body. The vertebral arch is attached to the body with the help of two pedicles of vertebral arch, pediculi arcus vertebrae, thus bounding the vertebral foramen, foramen vertebrale (fig. 2.1).
The foramina of all vertebrae form the vertebral canal, canalis vertebralis, enclosing the spinal cord. Openings for blood vessels named nutrient foramina, foramina nutricia, are visible on the surface of the vertebral body.
Seven processes project from the vertebral arch. An unpaired spinous process, processus spinosus, projects dorsally along the median line. The paired transverse processes, processus transversus, project on the right and on the left in the frontal plane. The paired superior and inferior articular processes, processus articularis superior et processus articularis inferior, project up and down from the arch. The bases of the articular processes bound the superior and inferior vertebral notches, incisura vertebralis superior et incisura vertebralis inferior. The inferior notches are deeper than the superior ones. When the vertebrae are articulated with each other, the inferior and superior notches form an intervertebral foramen, foramen intervertebrale, on the right and on the left. The intervertebral foramina transmit spinal nerves and blood vessels.
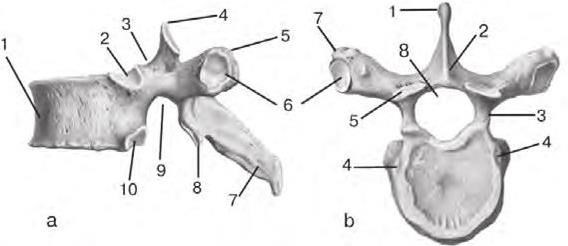
Fig. 2.1. Thoracic vertebra:
a – lateral aspect: 1 – vertebral body (corpus vertebrae); 2 – superior costal demi-facet (fovea costalis superior); 3 – superior vertebral notch (incisura vertebralis superior); 4 – superior articular process (processus articularis superior); 5 – transverse process (processus transversus); 6 – transverse costal facet (fovea costalis processus transversi); 7 – spinous process (processus spinosus); 8 – inferior articular process (processus articularis inferior); 9 – inferior vertebral notch (incisura vertebralis inferior); 10 – inferior costal demi-facet (fovea costalis inferior)
b – superior aspect: 1 – spinous process (processus spinosus); 2 – vertebral arch (arcus vertebrae); 3 – pedicles of vertebral arch (pediculi arcus vertebrae); 4 – superior costal demi-facet (fovea costalis superior); 5 – superior articular process (processus articularis superior); 6 – transverse costal facet (fovea costalis processus transversi); 7 – transverse process (processus transversus)
2.2. Cervical Vertebrae
The cervical vertebrae, vertebrae cervicales (CI– CVII), form the upper (cervical) part of the vertebral column. Two upper cervical vertebrae of seven significantly differ from other ones, therefore, they are termed atypical vertebrae. We will study them later. The other five vertebrae are structured according to the general principle: their bodies are relatively small, have an ellipsoid form, the vertebral foramen is large and triangular.
The distinctive feature of all cervical vertebrae is the presence of transverse foramina, foramen transversarium, in the transverse processes. They are formed as a result of the fusion of the transverse processes and the rudiments of the cervical ribs. The vertebral artery and vein pass through these foramina.
The groove for spinal nerve, sulcus nervi spinalis, passes along the superior surface of the transverse prosesses of the III–VII cervical vertebrae. These processes end with two tubercles – anterior and posterior, tuberculum anterius et tuberculum posterius. The anterior tubercle of the VI vertebra is more developed than the anterior tubercles of other cervical vertebrae. It is termed carotid tubercle, tuberculum caroticum, because the carotid artery can be compressed to it during hemorrhage.
The spinous processes are short and directed downwards, and their ends are bifurcated. The spinous process of the VII cervical vertebra is the longest, and its end is thickened. This vertebra is called prominent, vertebra prominens, because the apex of its spinous process is clearly palpated in a living person.
The articular processes of the cervical vertebrae are short and located obliquely between the frontal and horizontal planes. Meanwhile, the superior articular processes are directed backwards and slightly upwards, the inferior articular processes are directed forwards and slightly downwards (fig. 2.2).
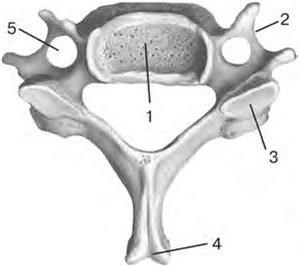
Fig. 2.2. Typical cervical vertebra (superior aspect):
1 – vertebral body (corpus vertebrae); 2 – transverse process (processus transversus); 3 – superior articular process (processus articularis superior); 4 – spinous process (processus spinosus); 5 – transverse foramen (foramen transversarium)
The shape of the first two cervical vertebrae is influenced by their close location to the skull. They are involved in head turning. Therefore, they are termed «rotational vertebrae».
The I cervical vertebra is called the atlas, atlas (CI). It differs from the general structure of individual vertebrae: it has no body no notches and no spinous or articular processes (fig. 2.3).
The atlas has an anterior arch, arcus anterior atlantis, instead of the body. Its anterior surface has an anterior tubercle, tuberculum anterius; on its posterior surface there is a small articular facet, fovea dentis, with which the II cervical vertebra is joined.
The lateral masses of atlas, massae laterales atlantis, are located on the both sides. Each of them bears an ellipsoid, concave superior articular surface, facies articularis superioris, joining with the corresponding occipital condyle. The inferior articular surfaces, facies articulares inferiores, form round, slightly concave articulate areas connected with the II cervical vertebra.
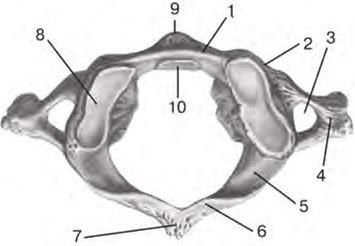
Fig. 2.3. I cervical vertebra (atlas) (superior aspect):
1 – anterior arch of atlas (arcus anterior atlantis); 2 – lateral mass (massa lateralis); 3 – transverse foramen (foramen transversarium); 4 – transverse process (processus transversus); 5 – groove for vertebral artery (sulcus arteriae vertebralis); 6 – posterior arch of atlas (arcus posterior atlantis); 7 – posterior tubercle (tuberculum posterius); 8 – superior articular surface (facies articulars superior); 9 – anterior tubercle (tuberculum anterius); 10 – facet for dens (fovea dentis)
The posterior arch of the atlas, arcus posterior atlantis, corresponds to the arch of a typical vertebra. There is a reduced spinous process in the form of a small posterior tubercle, tuberculum posterius, on the back surface of the posterior arch. The groove for vertebral artery, sulcus arteriae vertebralis, passes on the superior surface of the posterior arch behind the lateral mass.
The vertebral foramen, foramen vertebrale, is bounded with arches and lateral masses. It is much larger than the vertebral foramina of other vertebrae, and only its posterior part corresponds to them. In its anterior part narrowed on the sides with the lateral masses, the dens of the II cervical vertebra is located. The transverse process, рrocessus transversus, is perforated by the transverse foramen, foramen transversarium, for the passage of blood vessels like transverse processes of the other cervical vertebrae. The ends of the transverse processes are slightly thickened. They have no anterior and posterior tubercles and no the groove for spinal nerve.
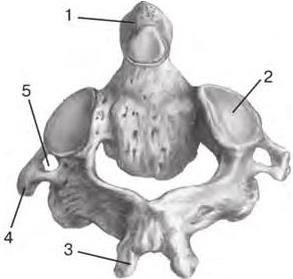
Fig. 2.4. II cervical vertebra (axis) (posterior aspect):



